by Ben Taylor
First cases of Covid-19 in Tanzania
[Editor’s note: As this is a fast-changing situation, the details provided here are likely to be somewhat out of date by the time this issue reaches readers. Nevertheless, every effort has been made to ensure the details were correct at the time of writing (April 24).]
The first recognised case of Covid-19 in Tanzania was recorded on March 16 in Arusha, a Tanzanian woman who had recently returned from Belgium. Two further cases were recorded two days later, one in Dar and the other in Zanzibar, both foreign nationals. Three more followed the day after that.
The government acted swiftly, closing all schools with immediate effect on March 17 and universities from the following day. Major sporting events were also suspended. A contact-tracing and testing system – designed with a potential Ebola outbreak in mind – was put in place.
Nevertheless, the number of cases crept upwards over the following days and weeks. The first death was recorded on March 31.
Initially, cases were limited to those having recently arrived in the country from countries where the outbreak was already more widespread. However, on April 9, the Minister of Health, Ummy Mwalimu announced that the first recorded case of local transmission had been detected around the start of the month.
At the time of writing, the number of recorded cases has begun to rise more quickly, reaching 284 cases and ten deaths as announced by the government on April 22, up from 32 cases ten days earlier.
As has been the case across much of the world, the government has struggled to find the right response to an unprecedented and overwhelmingly difficult situation.
Even before the first cases were recorded in Tanzania, the President and the Minister of Health had both begun urging Tanzanians to take precautions – handwashing with soap, social distancing where possible and refraining from handshakes.

Maalim Seif Sharif Hamad (left) and President Magufuli tap feet in greeting on March 3rd – photo State House
President Magufuli himself set a public example when meeting with opposition leader Maalim Seif Sharif Hamad (of ACT Wazalendo) on March 3: rather than shake hands, they tapped feet. The photo featured prominently in news coverage, and did much to raise public awareness of the virus.
On March 13, the President urged the media to dedicate time alongside their news coverage to educate the public about the virus.
More substantive policy measures, however, have been more piecemeal. After the closure of schools and universities, the next major policy response came on March 23, when it was announced that all international arrivals into Tanzania from Covid-19-affected countries would have to undergo 14 days quarantine in designated hotels (at their own cost). This prompted distress from many returning Tanzanian citizens, who complained that the designated hotels were tourist-class hotels at prices beyond anything they would usually pay.
Three weeks later, the Tanzania Civil Aviation Authority suspended all international commercial passenger flights to and from Tanzania until further notice, though in reality almost all such flights had already ceased operating due to restriction in other countries and measures taken by airlines for commercial reasons.
A faith-based response
The government also urged people to remain at home as much as possible, travel less on public transport and refrain from socialising. The message was somewhat undermined, however, by repeated public statements by the President and other national figures encouraging people to continue to attend their churches and mosques as normal, as the country needed their prayers.
The President, speaking while attending a Sunday service on March 22, said the virus was “satanic” and “it cannot survive in the body of Jesus. It will burn.”
This approach drew criticism both within and outside the country. Opposition leader, Zitto Kabwe, accused the government of “a lack of seriousness” and the President of being in “a state of denial.”
Nevertheless, the President doubled down on the message. Shortly before Easter he stated that “this is the time to build our faith and continue praying to God and not depending on facemasks. Don’t stop going to churches and mosques for prayers. I’m sure this is just a change of wind and it will go like others have gone.” And on April 16, the President called for three days of national prayer, saying God would protect Tanzanians from the virus.

Social distancing not in evidence at Palm Sunday mass in Full Gospel Bible Fellowship Church in Dar es Salaam
This earned the President a spot in a list of the “Notorious Nine” world leaders who “responded to the coronavirus with denial, duplicity and ineptitude,” compiled by a Canadian newspaper, the Globe and Mail. “Tanzania today remains the only country where the government has recommended church attendance as a way of combatting the virus,” the paper reported.
The Prime Minister, Kassim Majaliwa, has differed only a little in his stance. “Prayers in houses of worship are desirable,” he said, “but we also need to take necessary precautions.” He added, however, that as even wealthy countries have not been spared the pandemic, “it is time we sought divine intervention”.
On April 22, the President extended his advice a little beyond prayer
– to incorporate tradition medicine using steam inhalation. This, he said, was “scientifically very clear, because vapour is above 100 degrees centigrade and the virus will disintegrate,” before suggesting that concoctions made of Neem trees, onions and other ingredients could be beneficial, though without specifying whether as prevention or as treatment.
Scientists have concluded that this would have no positive effect, could cause burns and might make people more vulnerable to infection or to infections causing more severe problems. A Reuters fact check (not responding to President Magufuli, but to earlier online posts claiming steam inhalation as a cure), concluded that the idea was false, and indeed dangerous. Similarly, a BBC factcheck concluded that “any attempt to inhale steam at this temperature, would be extremely dangerous … and your lungs would certainly be irreparably damaged before reaching a temperature high enough to deactivate the virus.” Scientifically, it is very clear.
After making this suggestion, the president concluded that “we will beat Corona by working together, by putting an end to fear, by putting God first, and will beat Corona as we have been able to win other wars.”
No lockdown, “never”
The President has also shunned all calls for a lockdown. “Let us continue working hard to build our nation,” he said in mid-April. “Coronavirus is not and should not be a reason for us not working. Farmers should utilise the ongoing rains effectively, industrial owners should continue producing and I don’t expect any development project to stop.”
Some minimal social distancing measures were put in place. In addition to the closure of schools, universities and sporting events, this includes attempts to prevent overcrowding on public transport – no more passengers permitted than the number of seats – and some restrictions (later relaxed) on travel between Dar es Salaam and up-country locations. Many rural communities have put in place their own measures to fine or quarantine anyone arriving from Dar es Salaam – as many have done, recognising the lower risk associated with lower population densities and the possibility of growing your own food. The April 26 Union Day public celebrations have been cancelled, as has the Uhuru Torch race.
Opposition leaders say the country needs to take more urgent action to avoid potential disaster. Freeman Mbowe, the chairman of the largest opposition party, Chadema, posted on Twitter: “No lockdown because he (President Magufuli) wants to save the economy and his flagship infrastructure projects. The lives of our people cannot be repaired but the economy can! Lockdown or get locked out!”
The President has repeatedly resisted all such calls. On April 22, speaking in his hometown of Chato to security force leaders, he addressed the issue again: “There are those who have suggested that we lockdown Dar es Salaam. This is not possible,” he said. “Dar es Salaam is where we collect almost 80 per cent of the country’s revenue, we can continue taking measures to curb the virus but not by locking down Dar es Salaam. Never!”
At the time of writing, the truth is that social distancing has not become part of life for many in Dar es Salaam or other urban areas of Tanzania. Markets, public transport and bars remain crowded, as well as places of worship.
And the government faces some impossible choices in this regard. While a small number of Dar es Salaam residents – primarily those in middle class jobs – are able to work from home, the reality for many is that this would spell rapid and severe economic distress. Tanzania lacks the economic capacity to provide either direct financial assistance or food aid to the millions who would need it.
There is considerable debate about whether a lockdown might not be the best response in many African countries, where populations are both extremely young and financially vulnerable. Melissa Leach, the Director of the Institute for Development Studies (IDS) and James Fairhead, an environmental and medical anthropologist, both at the University of Sussex, have written that “the best policies for countries with young populations may not be lockdowns.”
Around 3% of Tanzania’s population is aged 65 or above, compared to around 18% in the UK and 20% in Italy.
“There may be better ways to save lives such as physically shielding and supporting the most vulnerable while allowing the wider population to gain immunity, whether through a vaccine when it arrives or by virtue of enough people catching and recovering from the virus itself,” they wrote. “Poor countries are much less able to cushion the potentially devastating economic impacts produced by lockdowns. This is if they are feasible in the first place. Effective lockdowns are near impossible in crowded low-income settlements that lack taps and sewers.”
“Today, some version of the lockdown has become most countries’ response to the Covid-19 pandemic. In years to come, we may look back on this moment as one in which an ideological practice emanating from older and wealthier countries was misguidedly “copy and pasted” by elites in younger and poorer societies, leading to marginal benefits in tackling the coronavirus but with the effect of increasing poverty and mortality among the poor.”
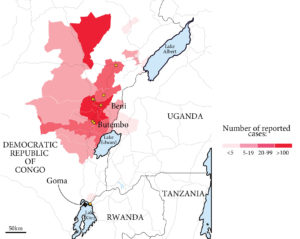
Nevertheless, most of Tanzania’s neighbours have opted for forms of lockdown that go well beyond anything being done in Tanzania. In Uganda, the country has been in strict lockdown since March 30. Movement is restricted, public gatherings are suspended and all but a small number of essential businesses are closed. This is enforced in Kampala and other urban centres by a heavy police presence on the streets. In Kenya, the government has not gone quite so far, though did introduce a nationwide 7pm-5am curfew and the closure of all bars and restaurants in late March, followed by a ban on movement in and out of Nairobi and other major urban centres in early April.
Health services
Much of Tanzania’s epidemic preparations have been with Ebola in mind, with contact tracing and testing and isolation of patients of a relatively small number of patients. It is not designed to cope with the large numbers of patients the current pandemic has seen around the world, nor with asymptomatic carriers.
The number of ventilators available is low (the precise number is unknown), stocks of protective equipment for health workers are minimal, even supplies of running water and electricity are unreliable in many hospitals. Five hundred ventilators were donated by Chinese entrepreneur, Jack Ma, on April 8, and several local business figures have donated masks, gowns and other equipment. Doctors have complained about a shortage of protective equipment.
Initially, all positive Covid-19 cases in Tanzania were being isolated in selected hospitals, including those with few or no symptoms. Since April 19, this is primarily the Amana Hospital in Ilala, Dar es Salaam. All other patients at the hospital were transferred elsewhere. Muhimbili National Hospital has been directed to refer all Covid-19 patients to Amana, and to focus exclusively on other medical needs. There have been some efforts to increase capacity at Amana and supply it with new equipment.
There have also been reports of unrest among patients in isolation at Amana. On April 24, it was reported that some patients had staged a breakout. Different reports stated this was either due to dissatisfaction at the poor standard of care being provided to more serious cases or due to frustration among patients with no symptoms that they were being kept for an unnecessarily long time against their will. Similar events were seen the same day in Nairobi, Kenya.
International support, and concern
Various donor agencies have pledged additional financial assistance to Tanzania to cope with the pandemic, though details in most cases are scarce. The government of Ireland responded very quickly, providing €1.5 million to support the national response seven days after the first case was announced. Tanzania has been promised part of a €1.2 billion package set up by the French government to support Covid-19-responses across Africa. The British government has pledged some direct support to Tanzania (“an initial” £2.7 million), but has put large amounts toward international efforts towards vaccine development (£544 million) and the work of international agencies (£200 million) including the World Health Organisation (WHO), UNICEF and the World Food Programme in combatting the pandemic. The EU has raised over €15 billion to support the global response, though this is likely to focus most on supporting economic mitigation and recovery. The US government has committed around $1.5m towards the Tanzanian response.
On April 22, President Magufuli thanked the World Bank for making loans available for financing the response, but suggested that the Bank should instead cancel debts owed by Tanzania and other developing countries. “Now is the right time for the World Bank, which has been touched by the crisis and has good intentions to assist us, to forgive part of the debts we owe, so that the money we are paying each month, and the interest, can be put towards responding to the Coronavirus crisis. This is my request, and I request also that other African countries should join in this call.

WHO Regional Director for Africa Matshidiso Moeti who also urged countries not to let Covid-19 eclipse other health issues.
On April 24, the WHO Regional Director for Africa Matshidiso Moeti said there were concerns about the rise of cases reported in Tanzania in the previous few days. “Certainly in Tanzania we have observed that physical distancing, including the prohibition of mass gatherings, took some time to happen and we believe that these might have been probable factors that led to a rapid increase in cases there.”
Uncertainty and trepidation
The coming months hold a high level of risk and uncertainty for the whole world, with every country facing its own unique challenges according to the local context – and a degree of luck. For Tanzania, it now seems unlikely that the outbreak will be contained, and therefore probable that the virus will spread rapidly in low income neighbourhoods of Dar es Salaam, as well as other towns and cities. It seems unlikely that health services will be able to respond effectively. And it seems likely that the economic consequences – lockdown or no lockdown – will be severe for many, with urban areas again likely to be hardest hit.
Lower population densities in rural areas may offer some protection – both reducing the chance of infections reaching rural communities and slowing the spread within such areas. In rural areas, households are also more likely to be able to produce a greater proportion of the food they need. The young age of the population may offer some protection, if fewer of those who contract the virus suffer severe symptoms, though this may also contribute to faster spread among asymptomatic carriers.
The truth is, however, that this situation is unprecedented in modern times. Nobody truly knows how it will play out, nor what the cost in lives will be, nor the impact on food security and the wider economy.